INTRODUCTION
Schizophrenia affects around 0.3–0.7% of people at some point in their life or 21 million people worldwide as of 2011.[1] Estimates of the international prevalence of schizophrenia among non-institutionalized persons, are 0.33%–0.75%.[2] The vast majority of people with schizophrenia responds to treatment and live normal lives in the community. Statistics on people 10 years after their initial psychotic break include that 25% of people have experienced recovery, 25% are much improved and living independently, 25% are improved but require constant support, children and people over 45 rarely get schizophrenia, 15% are hospitalized, and 10% are dead mostly of suicide.[3]
Schizophrenia treatment based on the dopamine hypothesis has been successful. However, despite many decades of effort by both scientists and drug companies, all currently available clinical treatments still primarily target the dopamine D2 receptor. The reason behind this inconvenient result may be due to the heterogeneity of psychosis. Patients with schizophrenia exhibit marked variations in symptoms, even the biological characterization of symptom domains of schizophrenia remains unclear, and the responses to different therapeutic interventions also vary significantly.[4]
By 2020, schizophrenia will most likely still be a clinically defined primary psychotic disorder. While there is some hope that treatment will be improved with new antipsychotic drugs, drugs addressing negative symptoms, more refined psychotherapy approaches, and the introduction of new treatment modalities such as transcranial magnetic stimulation, an additional hope is to improve early detection and prevention. As the results of new research into the etiopathogenesis of schizophrenia are promising to improve diagnosis, classification, and therapy in the future, a picture of complex brain dysfunction is currently emerging requiring sophisticated mathematical methods of analysis.[5]
The negative attitudes were found to be associated with the previous and current experience of side effects, experience of stigma, the nature of the tendency to stop medication, and misconceptions about medication.[6] Studies have found that 25%–80% of all schizophrenic patients are non-compliant in medication-taking. Non-compliance of medication-taking is associated with higher readmission rates that result from relapses.[7]
One of the study findings suggests that insight toward mental illness is also poorly associated with adherence to treatment and drug compliance. Subjective acceptance of antipsychotic medications is higher for inpatients, but average number of subjects have shown a negative attitude toward antipsychotic medicine because confounding factors overshadowed the real problem they encountered.[8] Patients on second-generation antipsychotics (SGAs) had more positive views of their medications than those on first-generation antipsychotics. Positive attitudes toward antipsychotics were common among patients with schizophrenia. Patients on SGAs had better attitudes, possibly because of less severe side-effects and greater insight among them.[9]
Two studies compared compliance therapy to standard care, and both found compliance therapy to significantly improve drug attitude.[7] The systematic review identified several interventions that can improve patients’ compliance in mental health treatment, for example, adherence therapy and motivational interviewing techniques during in-hospital stay. Conclusions were drawn and recommendations formulated for nursing practice, education, and research.[10]
Compliance therapy has been developed to modify negative beliefs toward medication and aims to improve drug attitude toward medication-taking. However, the effect of compliance therapy on drug attitude among schizophrenic patients is unclear. The majority of studies identified an effect of compliance therapy in improving drug attitude. However, the evidence is still weak as the outcome was from three small heterogeneous studies. Standardization of the compliance therapy and well-designed study is needed to test the effect in the future. Only then, the therapy can be considered to improve attitude toward medication-taking among schizophrenic patients.[7]
Paucity of research literature on compliance therapy for drug attitude initiated the investigator to conduct the present study. The novelty of the research work is on compliance therapy for drug attitude among schizophrenic patients.
MATERIALS AND METHODS
After obtaining written informed assent/consent, schizophrenic patients who fulfill the inclusion criteria were recruited and enrolled in the study on April 2018. The total sample size was 50, of which 25 were in experimental group and 25 in control group. Purposive sampling technique was adopted in this study.
Schizophrenic patients with intellectual insight and true emotional insight (Clinical Rating of Insight-6 point scale) were selected in the experimental and control groups. Participants were randomly allocated using random number table either to experimental group or control group.
All participants were interviewed before intervention by assessing background variables such as age, education, religion, marital status, family monthly income, type of family, residence, duration of illness, and family history of mental illness. The level of drug attitude was assessed using Drug Attitude Inventory-10.
Immediately after pre-test, experimental group received compliance therapy. Compliance therapy comprises of the following sessions
-
Session I - Introduction, review history of illness and benefits, and drawback of the drugs in the treatment
-
Session II - Stigma in drug treatment
-
Session III - Focusing on symptoms and adaptive behavior
-
Session IV - Self-efficacy and adherence to drug treatment
Session I was administered during the 1st week, Session II was administered during 2nd week, Session III was administered during 3rd week, and Session IV was administered during 4th week. Experimental group received compliance therapy for 4 weeks, with duration of 30–40 min. Session I was conducted in person (face-to-face confrontation), followed by Sessions II, III, and IV were conducted through telephone mode on weekly basis (twice a week). Control group received standard methods of care.
Post-test was conducted on the 4th week using the same assessment techniques in the course of review. Pre- and post-test were conducted in-person both in experimental and control groups.
RESULTS AND DISCUSSION
In pre-test, experimental group showed that highest 48% of the subjects had neutral attitude toward the drug, and in post-test, majority 44 % of subjects showed neutral attitude toward the drug. In pre-test, control group showed that paramount 40% of the subjects had neutral attitude towards the drug, and similarly in post-test, highest 40% of the subjects had neutral attitude toward the drug. These findings were inconsistence with the research report of schizophrenic patients who had predominantly positive attitudes toward antipsychotics.[9]
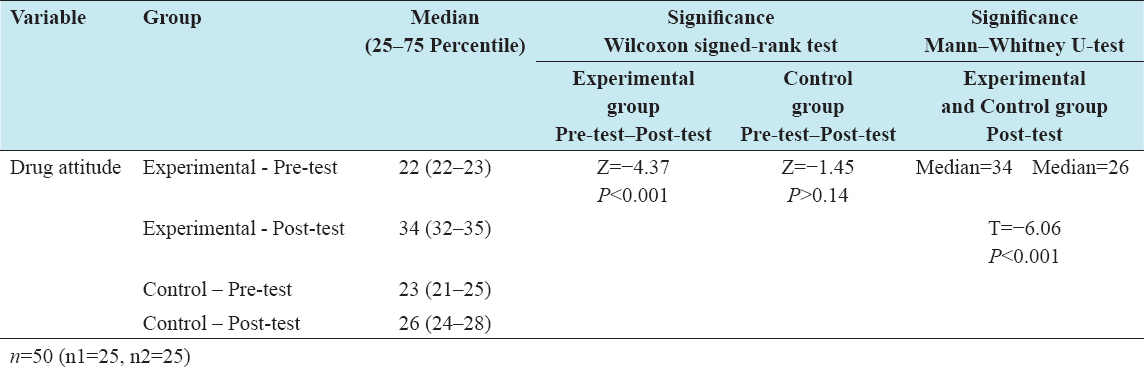
Comparison of the median of pre-test drug attitude scores in experimental group showed 22 and post-test showed 34. Likewise, a comparison of the median of pre-test drug attitude scores in control group showed 23 and post-test showed 26.
Wilcoxon signed-rank test scores within the experimental group (pre-test and post-test) showed statistical significance (Z = −4.37) with negative differences on drug attitude. Non-significant (Z = −1.45) negative differences were shown within the control group while computing the drug attitude. Similarly, Mann–Whitney U-test (between experimental and control groups) showed statistical significance (T = −6.06) with negative differences in post-test scores on drug attitude. It indicates that there was a significant difference between the groups. Based on post-test drug attitude median scores, experimental group (median=34) showed improvement in drug attitude compared with control group (median=26) [Table 1].
Table 1: Comparison of median, Wilcoxon signed-rank test, Mann–Whitney U-test value with pre- and post-test scores of drug attitude between experimental and control groups
These findings were backing the research work of two studies which compared compliance therapy to standard care, and both found compliance therapy to be statistically significant in improving the drug attitude.[7]
Similar findings have reported statistical significance of compliance therapy on drug attitude among Chinese samples with Wilcoxon signed-rank test scores of −4.53 in experimental group and −3.60 in control group and Mann–Whitney U-test showed statistical significance (−1.30).[11]
A significant association was obtained between post-test drug attitude scores and duration of illness (χ2 = 6.00; significant) in experimental group, likewise significant association was obtained between post-test drug attitude scores and family history of mental illness (χ2 = 3.88; Significant) in control group. This finding was supported and affirmed that the lack of insight, the presence of more severe negative and depressive symptoms, and disease duration <5 years correlated significantly with negative attitudes toward antipsychotic medication.[12]
CONCLUSION
The study findings revealed that administration of compliance therapy was highly significant to improve drug attitude among schizophrenic patients in the experimental group. There was no statistically significant evidence on the improvement of drug attitude among schizophrenic patients in control group.